What is diabetic foot?
Diabetic foot is a serious complication associated with diabetes. It occurs when high blood sugar levels are maintained over a long period of time, damaging the nerves and blood vessels in the feet.
This nerve damage gradually reduces sensation, so the person may no longer feel pain, heat or cold. As a result, minor injuries such as cuts, blisters or scratches can go unnoticed.
At the same time, poor circulation slows the healing of these wounds. Over time, these injuries can turn into chronic ulcers, open wounds that can persist for weeks or months if not treated properly.
When a wound remains open, the risk of infection rises. In severe cases, infection can lead to gangrene, i.e. tissue death. In such cases, amputation of a toe, foot or part of the leg may be necessary to stop the infection from becoming life-threatening.
Why does diabetic foot develop?
Diabetes is a condition in which blood sugar levels are higher than is healthy. Over time, this excess sugar can damage nerves and affects blood circulation.
The combination of loss of sensation and poor blood flow creates a vicious cycle: injuries go unnoticed, and when they do occur, the body struggles to repair them. Often, the process progresses silently, without pain, until the problem becomes severe.
Diabetic neuropathy: when the alarm system fails
The nervous system acts like the body’s natural alarm system. When faced with a painful stimulus, such as stepping on a stone or wearing tight shoes, the nerves send a signal to the brain prompting a reaction that protects the foot.
In people with diabetes, excess glucose can damage these nerves. This condition, known as diabetic neuropathy, causes numbness, tingling and loss of sensation.
When pain is not detected, a person may not realise they have a wound, blister or injury caused by footwear. Without treatment, the injury tends to worsen progressively.
Poor circulation makes wounds worse
Diabetes can also affect the arteries and blood vessels, causing them to harden and narrow. This condition is known as peripheral arterial disease.
Blood carries oxygen and the body’s natural defence, both of which are essential for wound healing. When blood flow to the feet is reduced, wounds heal slowly or may not heal at all. This causes the wound to remain open, creating an environment that is favourable for bacterial growth.
What are the stages of diabetic foot?
Diabetic foot rarely starts with a serious injury. In most cases, it develops gradually through a series of stages:
- Initial injury: a small cut, blister or callus forms, putting pressure on the skin. Due to loss of sensation, the person does not feel pain and does not take action.
- Ulcer: the skin breaks, creating an open wound that heals slowly or sometimes not at all. An ulcer that does not improve within one or two weeks is a high-risk warning sign.
- Infection: bacteria can enter through the ulcer. Poor circulation prevents the body’s defences from working effectively, allowing the infection to spread to deeper tissues and even the bone.
- Gangrene: if the infection is severe or blood flow is blocked, the affected tissue no longer receives oxygen and dies. The skin may darken and emit a foul odour.
- Amputation: when infection or gangrene threatens to spread, it may be necessary to amputate a toe, the foot or part of the leg to protect the person’s life.
Prevention is key
Most severe cases of diabetic foot can be prevented with proper and consistent care. The main recommendations are:
- Check your feet daily for cuts, blisters, redness or swelling.
- Wash your feet every day with lukewarm water and dry them thoroughly, especially between the toes.
- Wear comfortable, protective footwear and avoid walking barefoot.
- Trim your nails carefully and consult a podiatrist if you have ingrown nails or calluses.
- Maintain good blood sugar control.
Additional recommendations:
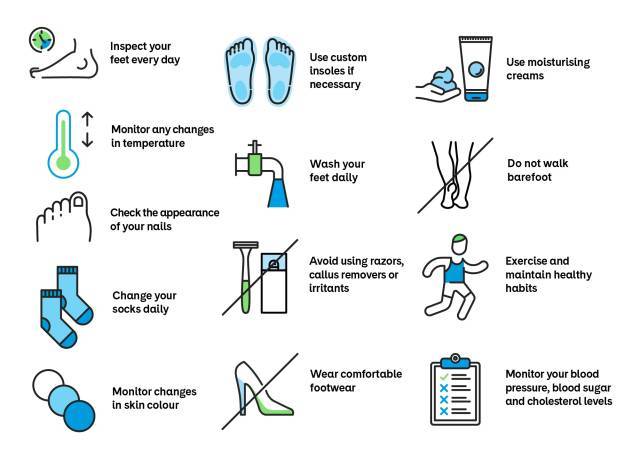
Fig.1: Recommendations for preventive diabetic foot care
Treatment of complicated diabetic foot
When ulcers or infections are present, treatment must be immediate and coordinated by a multidisciplinary team. It may include:
- Cleaning and dressing the wound, often using specialised materials that promote healing.
- Antibiotic treatment if infection is present.
- Offloading the foot to reduce pressure on the affected area, using specific devices or rest.
- Revascularisation: in cases of poor circulation, blocked arteries may need to be opened through procedures such as angioplasty or surgery to allow the wound to heal.
- Surgery: severe injuries may require removal of damaged tissue, and in extreme cases, partial amputation.
Diabetic foot is a serious condition, but it is often preventable. Any wound on the foot of a person with diabetes should be assessed promptly by a healthcare professional. The sooner treatment begins, the greater the chance of avoiding complications and preserving the foot.
Information documented by:
Dr Vicenç Riambau, Head of the Angiology and Vascular Surgery Department