Alcohol-associated liver disease (ALD) is one of the leading causes of liver disease in the world. Despite such high prevalence, the therapeutic options are scarce and the mechanisms that explain its progression are still not well understood. One of the biggest obstacles to advancing in the knowledge and treatment of ALD is the lack of experimental models that faithfully reproduce all phases of the disease, especially the most advanced ones. Animal models, common in biomedical research, fail to imitate the complexity of the human liver affected by alcohol, which makes it difficult to develop new drugs.
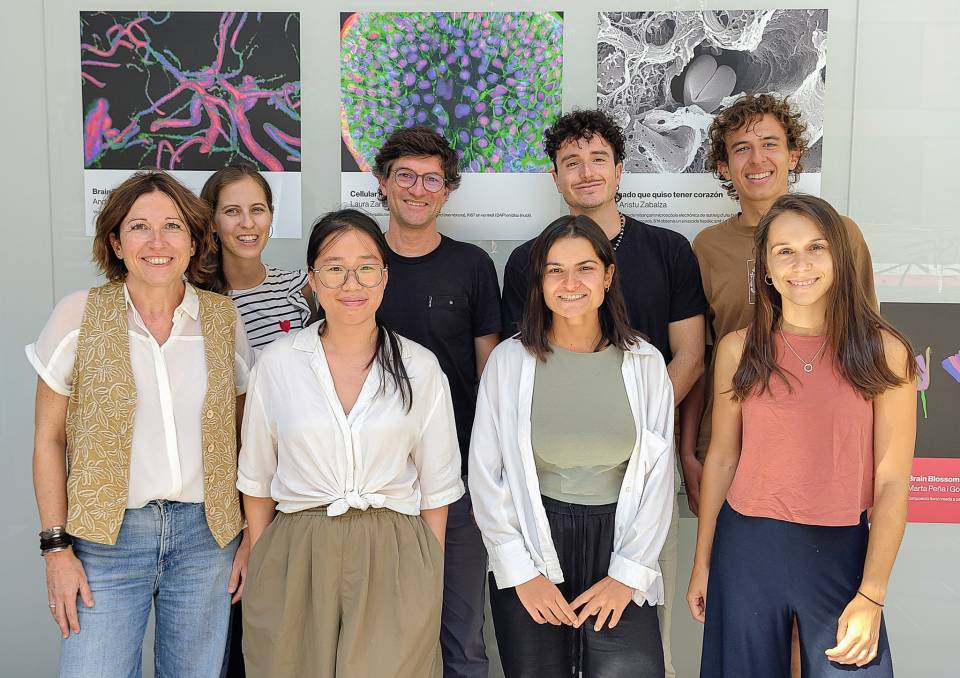
Faced with this challenge, a team of researchers led by Pau Sancho-Bru, Sílvia Ariño and Raquel Ferrer, from the IDIBAPS Liver cell plasticity and tissue repair research group ubicated at Esther Koplowitz Centre has developed a new technology that enables liver organoids to be developed from biopsies of patients at different stages of the disease. The study has been published in the Journal of Hepatology.
What are organoids and why are they important?
Organoids are small "mini-livers" grown in the laboratory from human cells. To date, the generation of liver organoids required samples obtained through surgical resections, an invasive procedure limited to patients in very advanced stages of the disease. Furthermore, these organoids were not able to reproduce the cellular diversity of the liver, especially the hepatocytes fraction, nor the complexity of the different stages of ALD.
The Journal of Hepatology study presents an innovative solution: the generation of organoids derived from needle biopsies (b-Orgs), a technique that allows samples to be obtained from patients at any stage of the disease. "These b-Orgs reflect the cellular composition of the human liver, including hepatocytes, bile cells and progenitors, and preserve the functional and molecular characteristics of each patient and each stage of the disease," explains Raquel Ferrer.
The team obtained liver biopsies from 62 patients with ALD, both in early and advanced stages. From these samples, they generated b-Orgs that were characterised using advanced techniques such as single-cell RNA sequencing and functional analysis. The results show that b-Orgs present a cellular heterogeneity that faithfully reproduces that of the human liver, and that they are able to model the progression of ALD in vitro.
In addition, b-Orgs respond to treatment with drugs such as prednisolone, demonstrating their potential as a tool for personalized medicine. This response capacity makes it possible to test the effectiveness of different treatments according to each patient’s characteristics, opening the door to a more targeted and effective therapy.
One of the study’s most relevant findings is the identification of the transcription factor ELF3 as a key element in cell plasticity and ALD progression. ELF3 activation is associated with hepatocyte dedifferentiation and worsening of the disease. This finding opens up new lines of research that may help to better understand the molecular mechanisms of ALD and to design therapeutic strategies aimed at this factor.
Implications for patients and the scientific community
The b-Orgs developed by the IDIBAPS team are a valuable tool for the study of liver diseases. "They make it possible to model the progression of ALD in a personalized way, identify new factors involved in the disease and test the effectiveness of drugs before applying them to patients. This can translate into better patient stratification, more accurate diagnosis and the development of more effective and safe therapies," adds Sílvia Ariño.
"This study shows that it is possible to overcome the limitations of animal models and of conventional organoids. Our goal now is to extend this methodology to other liver diseases, such as metabolic dysfunction-associated steatotic liver disease (MALSD), where variability between patients makes it essential to have reliable preclinical models, and to continue advancing towards more precise and effective medicine," concludes Pau Sancho-Bru.