17 June 2021
- What is it?
- Causes and risk factors
- Symptoms
- Diagnosis
- Treatment
- Living with the disease
- Progression of the disease
- Frequently Asked Questions
-
The disease at Clínic
-
Team and structure
Constipation diagnosis
Clinical history and physical examination
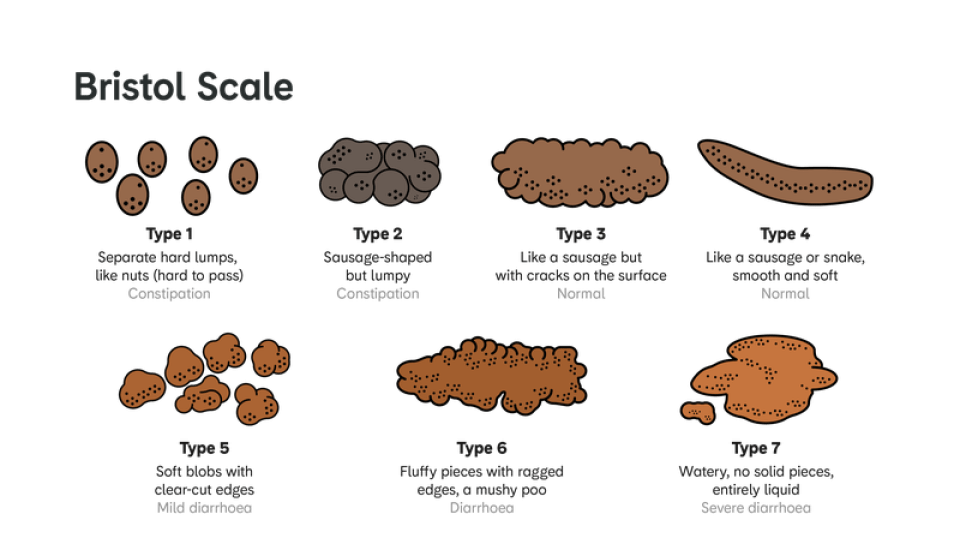
Clinical history and a physical examination are the most important aspects for evaluating a patient with constipation. It is essential to clearly understand the patient's discomfort, find out the duration of the symptoms and the general measures that the patient has taken to try and relieve this discomfort. The use of the Bristol scale (Figure), may be useful in allowing the patient to describe the shape and consistency of their faeces.
When considering medical history, three key aspects must be taken into account: 1) Detection of warning symptoms or signs, 2) Search for secondary causes of constipation, medication use, systemic or neurological diseases and local processes such as tumours, and 3) Compliance with the Rome IV criteria.
As part of a physical examination, a rectal inspection may provide a lot of information, as it allows anal diseases such as haemorrhoids, stenosis, fissures, rectocele or lumps to be detected. For example, asymmetry in the anal opening may suggest a neurological disorder affecting sphincter function, and failure of the perineum to descend when bearing down suggests pelvic floor dysfunction.
Warning signs
- Sudden change in the usual rhythm of bowel movements (for a period longer than six weeks) in people over 50 years of age.
- Presence of blood in the faeces.
- Anaemia or lack of iron.
- Unexpected weight loss.
- Family history of colon or rectal cancer or inflammatory bowel disease.
- Palpable abdominal or rectal mass.
Additional examinations

Analysis. There is no evidence that a general blood test is effective as a routine test in patients with constipation, although it is indicated in patients with warning signs and in those whose clinical history indicates constipation due to secondary causes. As part of the diagnosis investigation, some guidelines recommend a complete blood count with determination of serum iron (iron present in blood serum); an ionogram (blood electrolyte levels); serum calcium and phosphorus; glucose; and thyroid hormone levels, in addition to any specific tests deemed necessary based on the clinical suspicion of the disease causing the constipation.

Single-view abdominal x-ray. This can be very useful in the evaluation of hospitalised patients with acute constipation or with significant worsening of chronic constipation, especially when the physical examination suggests a possible obstruction or pseudo-obstruction. The radiograph may show various abnormalities: faecal impaction or faecaliths (accumulation of hard stool) in the distal region of the rectum; dilated bowel loops (in cases of mechanical or adynamic obstruction, such as Ogilvie's syndrome); or sigmoid colon volvulus (bowel obstruction caused by torsion of the sigmoid colon). It is not indicated in chronic constipation without warning signs, due to its limited diagnostic value.

Colonoscopy. A colonoscopy of patients with constipation as the only symptom provides similar results to the general population, so it is not recommended as a routine diagnostic test. However, it may be indicated in patients with warning signs, including the onset of symptoms after the age of 50. In these cases, a prior faecal occult blood test is recommended. Colonoscopy is also considered if laxative treatment fails.
Functional tests

Anorectal manometry. Manometry allows the function of the anal sphincter to be assessed at rest and during defecation, as well as the reflexive activation of the pelvic floor. This can measure rectal sensitivity and compliance, and relaxation of the external and internal anal sphincter. It is indicated in patients who do not respond to first-level hygiene and dietary measures or laxatives. It is useful in the diagnosis of functional defecation disorders and for the correct selection of patients who are candidates for rehabilitation treatment using anorectal biofeedback.

Balloon expulsion test. This consists of introducing a balloon in the rectum. It is filled with 50 ml of water that the patient must evacuate. Although the methodology for this test varies, the most common approach is to determine the time it takes for the patient to expel the balloon into the toilet. This test is indicated for patients who do not respond to treatment with lifestyle changes and first-line laxatives, and when constipation is suspected to be caused by a bowel movement disorder.

Determining colonic transit time (CTT). This is a very useful examination for patients suspected of having slow colonic transit as the cause of constipation. It is determined by ingesting small radiopaque markers made of a light plastic substance and then performing serial abdominal X-rays to quantify colonic transit time. The most commonly used protocol in Spain is to take X-rays at 4 and 7 days, and sometimes even on the 10th day. Excessive delay in the progression of these markers and their retention in the colon are indicative of a diagnosis of colonic inertia or colonic hypomotility. This test is indicated in patients who do not respond to treatment with lifestyle changes or first-line laxatives and when constipation is suspected to be caused by colonic hypomotility.

Video defecography. Defecography allows assessment of the anatomy and functional changes of the anorectum and is useful when anatomical causes of constipation, such as enterocele or intussusception are suspected, and in patients with pelvic floor dysfunction. It is considered an adjunctive test and, therefore, is not recommended as a sole examination for the diagnosis of these conditions. In this test, 150 ml of barium is inserted into the patient’s rectum. They are asked to perform Valsalva manoeuvres (coughing, pushing) and the elimination is monitored. There are two techniques for identifying anatomical abnormalities:
- Fluoroscopy. This has the advantage of being accessible and quick, but it is irradiating.
- MRI. This has the advantage of observing all the pelvic floor organs during defecation without irradiation, but it is expensive and less accessible than the first. Currently, the Clínic offers magnetic resonance defecography.
Substantiated information by:


Published: 21 July 2020
Updated: 24 July 2025
Subscribe
Receive the latest updates related to this content.
(*) Mandatory fields
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox