- What is it?
- Causes and risk factors
- Symptoms
- Diagnosis
- Treatment
- Evolution of the disease
- Living with the disease
- Research
- Frequently Asked Questions
-
La enfermedad en el Clínic
-
Equipo y estructura
What is diabetic retinopathy?
Diabetic retinopathy is an eye condition caused by diabetes. The blood vessels in the retina deteriorate and bleed or cause fluid to accumulate, which can lead to a loss of visual acuity and even blindness. The longer the history of diabetes, the greater the risk of developing diabetic retinopathy. It may or may not produce symptoms, so prevention consists of regular examinations of the eye fundus.
Diabetic Retinopathy explained in first person
The risk of developing diabetic retinopathy in patients who have had diabetes mellitus for more than 20 years is over 70%. It is the primary cause of blindness among adults of working age.
Monitoring your diabetes, that’s the most important thing. Everything helps, but you must monitor your diabetes.
Diabetic retinopathy is a secondary complication of diabetes which affects the back of the patient’s eye, i.e., the retina. Changes occur to the circulation in the retina’s blood vessels, this results in bleeding and accumulations of fluid. These problems can cause a loss of visual acuity, which in some cases may eventually lead to blindness.
Therefore, it is important to know that maintaining good control over diabetes from the onset of the disease is the best preventive strategy for delaying the appearance and/or reducing the extent of damage to the retina. By the same token, regular examinations of the back of the eye (fundus) are essential to help detect and treat small lesions and therefore prevent their escalation.
Some knowledge of the anatomy of the retina and the areas affected by the disease proves helpful when trying to understand diabetic retinopathy. The centre of the retina (the macula) produces our fine central vision and if it becomes damaged, as in the case of diabetic retinopathy with macular oedema, the patient will suffer significant vision loss. If, on the other hand, the disease does not affect the macula, that is, diabetic retinopathy without macular oedema, the patient’s vision only begins to deteriorate in the advanced stages and will have a worse prognosis.
This difference is very important because patients with diabetes who do not complain of vision loss must undergo regular eye examinations (screening tests with retinography) to detect the condition as soon as possible. As for patients who do experience vision loss, they should visit the ophthalmologist as they may have diabetic macular oedema and require treatment.
Either way, if the damaged blood vessels are detected early and treated with modern procedures, vision loss is prevented in most cases and some patients even benefit from improved vision.
Classification of diabetic retinopathy
Diabetic retinopathy is classified according to changes that develop in the eye fundus.
The condition is classified depending on the severity and extent of damage:
- Mild non-proliferative. Slight changes to the fundus of the eye.
- Moderate non-proliferative. Severe changes, but without affecting the entire fundus.
- Severe non-proliferative. Severe changes affecting all areas of the fundus.
- Proliferative. The appearance of new blood vessels and/or internal bleeding.
It is also classified depending on whether fluid has accumulated in the central part of the retina, in other words whether there is diabetic macular oedema:
- Without diabetic macular oedema.
- With diabetic macular oedema.
The first classification is very important because patients do not notice any loss of visual acuity until they develop more severe forms of retinopathy (proliferative). Patients with diabetes therefore receive regular check-ups of the eye fundus, normally with photography, to detect the presence and severity of the complication at the earliest opportunity. Nonetheless, the second classification is also important because patients with diabetic macular oedema will suffer vision loss from the outset which cannot be restored without the correct treatment.
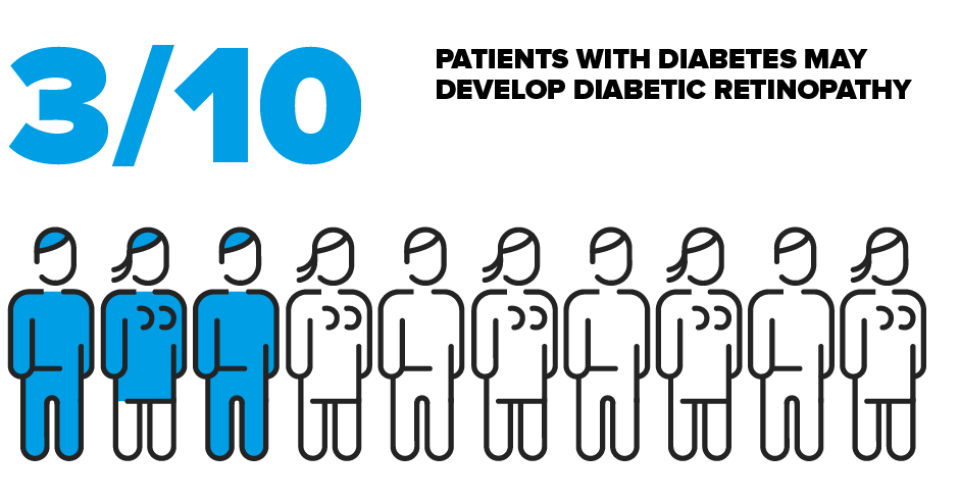
How many people are affected by diabetic retinopathy?
Diabetic retinopathy is the primary cause of blindness among people of working age worldwide.
On a different note, the longer the history of the diabetes, the greater the risk of developing diabetic retinopathy. That is to say, when diabetes is first diagnosed very few patients with type 1 diabetes and only a third of those with type 2 diabetes suffer from retinopathy. However, everyone with an extended history of diabetes (more than 20 years) may eventually develop retinopathy and it can ultimately affect as many as 6 out of 10 patients.
Related contents
Substantiated information by:


Published: 3 July 2018
Updated: 29 July 2025
Subscribe
Receive the latest updates related to this content.
(*) Mandatory fields
Thank you for subscribing!
If this is the first time you subscribe you will receive a confirmation email, check your inbox