Unit of Uro-Oncology Unit
The Uro-Oncology Unit at the Hospital Clínic de Barcelona is a model of excellence in the care of patients with urological cancer. Since its creation in 2011, the unit has stood out for its transversal structure, which integrates medical and surgical specialties, as well as complementary services that work in a coordinated manner to offer comprehensive, personalized and innovative care.
Vision and Objectives
The main objective of the Uro-Oncology Unit is to improve the quality of life of uro-oncology patients by providing care based on scientific evidence, technological innovation and the humanization of the care process. This translates into:
- The optimization of resources to ensure rapid diagnosis and high-precision treatment.
- The application of multidisciplinary protocols in all stages of the disease, including the initial and advanced stages.
- The continuous development of clinical and basic research to integrate advances in daily practice.
- The training of specialists in uro-oncology through reference teaching programmes.
Structure and Organization
The Unit is made up of a set of interconnected care and diagnostic areas that guarantee comprehensive and coordinated patient care.
Care area
- Urology: A comprehensive approach to patients with urological cancer, ranging from the initial diagnosis to surgical treatment and the management of advanced or metastatic disease. It includes advanced surgical techniques such as robot-assisted and laparoscopic surgery, as well as collaboration with other specialties in order to offer personalized multidisciplinary management.
- Medical Oncology: Specialized in systemic treatments, including chemotherapy, immunotherapy and targeted therapies, ensuring a response adapted to the needs of patients with advanced or metastatic cancer.
- Radiation Oncology: Advanced radiotherapy treatments such as stereotactic radiotherapy and hypofractionation are applied, allowing for precise localization and minimal side effects.
- Specialized nursing: Personalized patient support is offered, managing care pathways pre- and post-surgical education, and the monitoring of specialized care such as ostomies.
- Administration and management: Ensuring efficient patient registration, logistical coordination and administrative support in the care pathways.
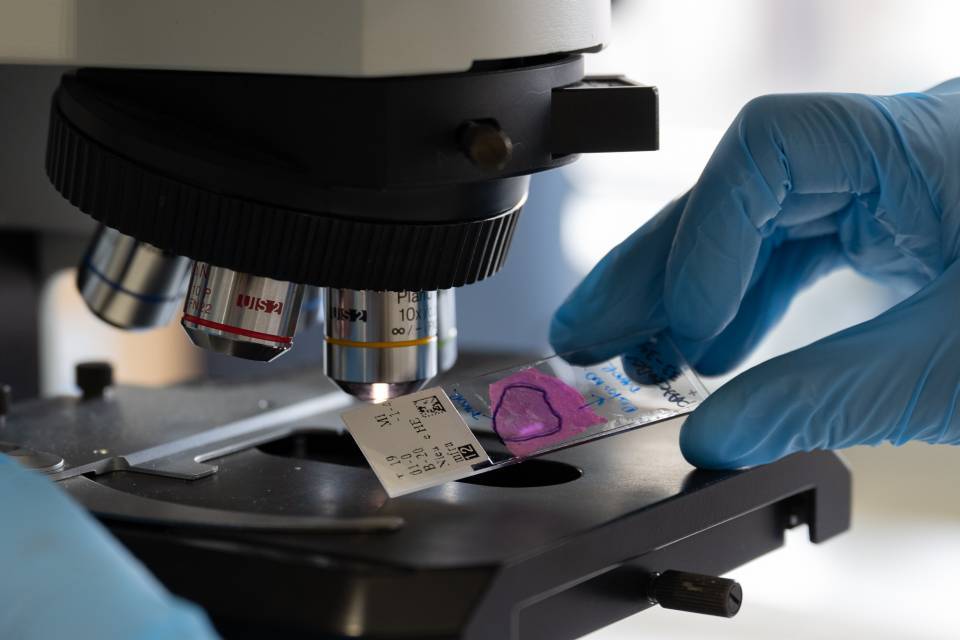
Diagnostic area
- Radiology and Nuclear Medicine: High-precision diagnostics with tools such as multiparametric MRI, PET-PSMA and advanced CT.
- Anatomical Pathology: Offering standardized reports that guarantee accurate clinical decision-making in line with international protocols.
- Rapid Diagnostic Pathways (RDP): Specialized programmes for early diagnosis and rapid initiation of treatment for prostate and breast cancer.
External collaboration
- Palliative and Geriatric Oncology: Providing comprehensive support to patients with complex needs derived from age or advanced stage of the disease, ensuring humanized and multidisciplinary care.
Distribution of roles
The leadership of the unit is shared between different disciplines:
- Head of Unit: Dr María José Ribal, with extensive experience in uro-oncology, minimally invasive surgery, research and teaching in the field of uro-oncology, as well as in the development of international clinical guidelines.
- Clinical coordinators: Specialists in each area of the unit (surgical, medical, radiotherapy, imaging, social work, pre-habilitation, nutrition, psychology).
- Nursing managers: Management and supervision of the care processes.
- “Core” group: Made up of key members who ensure strategic planning and adaptation to changing needs.
Technological Innovation
The Uro-Oncology Unit is distinguished by its constant commitment to technological innovation, integrating advanced tools and disruptive programmes in patient care. The main advances implemented include:
Diagnosis and Imaging
- Integration of PET-PSMA: This positron emission tomography technology with specific tracers has become essential for the staging and monitoring of prostate cancer. Its high sensitivity allows detection of disease at very early stages and improves the accuracy of treatment in oligometastatic patients.
- Multiparametric MRI: The diagnostic performance of magnetic resonance imaging for prostate cancer has been optimized, reducing inter-observer variability and improving the quality of PI-RADS reports.
- Predictive model for renal tumours: Development of advanced imaging techniques to differentiate between renal cell carcinomas and oncocytomas, with validation in clinical populations.
Advanced Surgical Techniques
- Robot-assisted surgery: Consolidation of the programme applied to muscle-invasive bladder cancer with the Enhanced Recovery After Surgery (ERAS) system, ensuring better postoperative results and shorter hospital stays.
Innovative treatments:
- Focal treatment in prostate cancer: Application of targeted ablations to treat only the affected areas of the prostate, reducing side effects and preserving the function of the organ. This technique represents a disruptive change with respect to traditional radical treatment.
- Advanced radiotherapy: The implementation of radiotherapy with moderate hypofractionation and extracranial stereotactic radiotherapy (SBRT) for the treatment of oligometastatic and localized cancer.
Molecular diagnosis support
- Molecular studies: Development of programmes to include molecular markers in healthcare practice, so as to personalize patient treatment even more.
- Liquid biopsy: Use of these techniques to monitor tumour progression in breast and prostate cancer.
Protocols and Standardization
The Uro-Oncology Unit of the Hospital Clínic de Barcelona stands out due to its rigorous application of protocols and standards in patient care. These protocols are based on the most up-to-date European clinical guidelines, ensuring that medical practice is aligned with the latest scientific evidence.
One fundamental component of this standardization is the Multidisciplinary Tumour Committee, which meets weekly to evaluate and discuss patient cases. This committee is made up of specialists in urology, medical oncology, radiation oncology, radiology, pathology, anatomical pathology, specialized nursing, and other health professionals. Its function is to review each case in detail, ensuring that therapeutic decisions are taken in a consensual and personalized manner, taking into account the particularities of each patient.
Commitment to Excellence
The Uro-Oncology Unit remains faithful to its commitment to offer high quality care, consolidating itself as a benchmark in the treatment of urological cancer and advancing towards new challenges in the fields of care, teaching and research.
Diseases, tests and procedures
Meet our professionals
The Unit is made up of a multidisciplinary team that promotes integrated care for uro-oncology patients. This team works together not only at the healthcare level, but also in teaching and research.